Cognitive Behavioural Therapy – CBT for Chronic Pain Across the UK and by Video Link.
If you are looking for a highly effective treatment for chronic pain or if you have been diagnosed with a medical problem that causes significant and persistent pain, Cognitive Behavioural Therapy can help. CBT is the recommended psychological treatment of choice for chronic pain and the independent research evidence demonstrates that it is fast and highly effective.
We know that chronic pain can be complex and highly debilitating. If you contact us to talk about your pain symptoms, we will listen to you and offer advice on how to best manage your pain symptoms without judgement or criticism. We understand that pain is highly individualised and experienced at an intensity that only the sufferer can fully appreciate. We will therefore only offer CBT for your chronic pain symptoms if we are confident that we can help improve pain management. Appointments start from just £85 with a BABCP-accredited CBT specialist and we can normally book an appointment within a few days of your initial enquiry. To book an initial call about CBT for pain management, complete the simple appointment request form on this page or email info@thinkcbt.com.
Online Cognitive Behavioural Therapy for Chronic Pain
As chronic pain can be highly debilitating, affecting posture and mobility, we provide CBT for chronic pain management online via video-link. The process works in exactly the same way as face-to-face therapy, with the added advantage of conducting CBT treatment sessions from the relative comfort of your own home. To find out more, email info@thinkcbt.com
What is Acute and Chronic Pain?
Pain is normally described as acute or chronic. Acute pain is normally experienced when the body is damaged or injured and when the initial healing process is underway. Chronic pain is usually experienced after a minimum period of three months and once the initial biological healing process has completed. Chronic pain is normally diagnosed when:
- The pain has continued for a period of three months or more following the healing process.
- The pain persists without a medical or physical cause or diagnosis.
- The intensity or frequency of pain increases with emotional distress.
- The pain interrupts the quality or quantity of your sleep.
- Pain medication is less effective, in spite of increased doses.
- The pain is affecting your home, social or work commitments.
- Key relationships have been affected by the pain.
- There is a marked increase in feelings of hopelessness about the future, helplessness to deal with the pain and a reduction in enjoyment.
- The pain causes increased irritability and you are finding it difficult to maintain an even temper.
If you are experiencing one or more of the above chronic pain symptoms, you can talk to us about undertaking CBT as a stand-alone approach or as part of an integrated pain management strategy. As we understand the complex links between biological and psychological factors, we can help you to manage your pain more effectively and significantly improve the quality of your personal and working life. We can also work on an integrated basis with physiotherapists, GPs, neurologists and other medical professionals to ensure a seamless approach..
How CBT is used to Treat Chronic Pain
Modern approaches to chronic pain management involve learning a range of cognitive and behavioural techniques to alter or alleviate pain symptoms. The CBT approach is based on a biopsychosocial model of pain management.
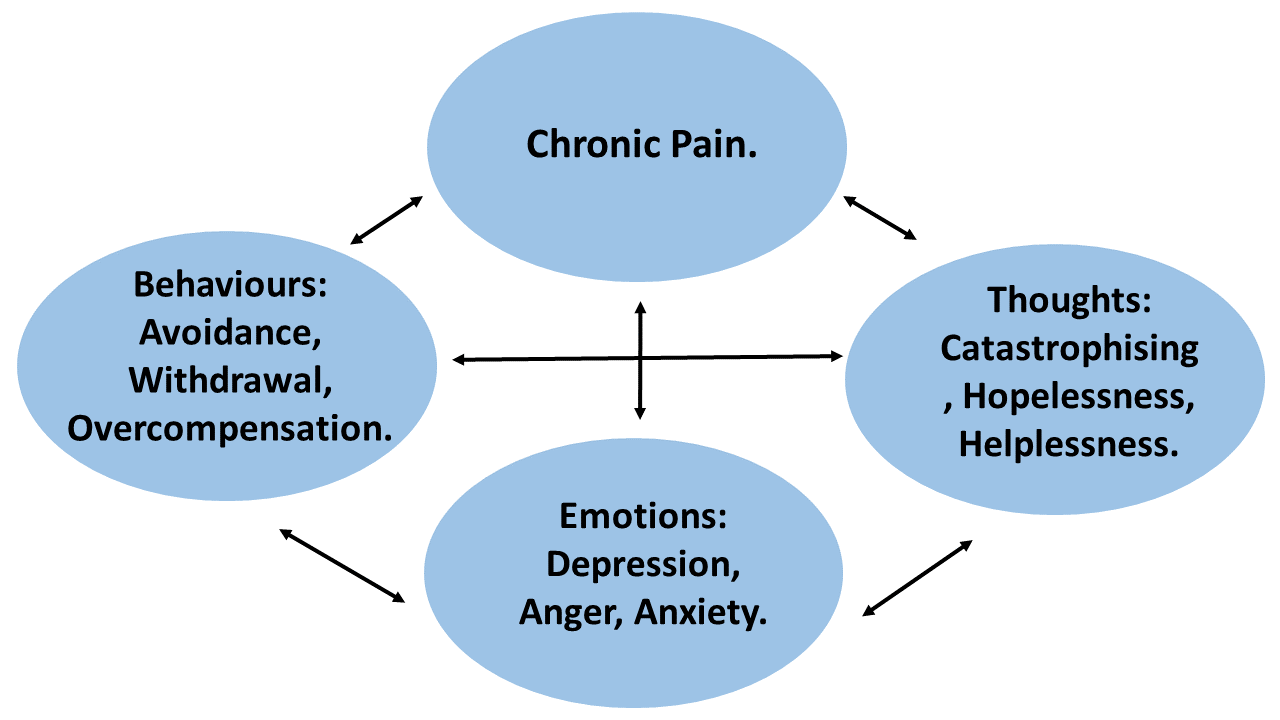
This recognises that chronic pain is maintained by emotional, cognitive, behavioural and context factors that influence the perception and intensity of the pain experience. CBT for chronic pain is theoretically informed by the Gateway Control model of pain perception and recognises the complex interplay between the peripheral and central nervous system.
Pain is triggered via the body’s sensory nerves known as nociceptors, channelled via a complex pain gateway in the spinal cord and experienced in different anatomical areas of the brain.
This means that psychological brain functions also significantly affect the way that pain is transmitted and experienced as suffering in the body. This mind-body connection is hard-wired via the nervous system and significantly amplified by emotional responses such as stress, anxiety, frustration, anger and depression. Empirical research has demonstrated that psychological factors including operant and conditioned learning, expectancy, memory, cognitive patterns, belief structures and anxiety / mood disorders all play a significant part in the individual’s subjective experience of pain.
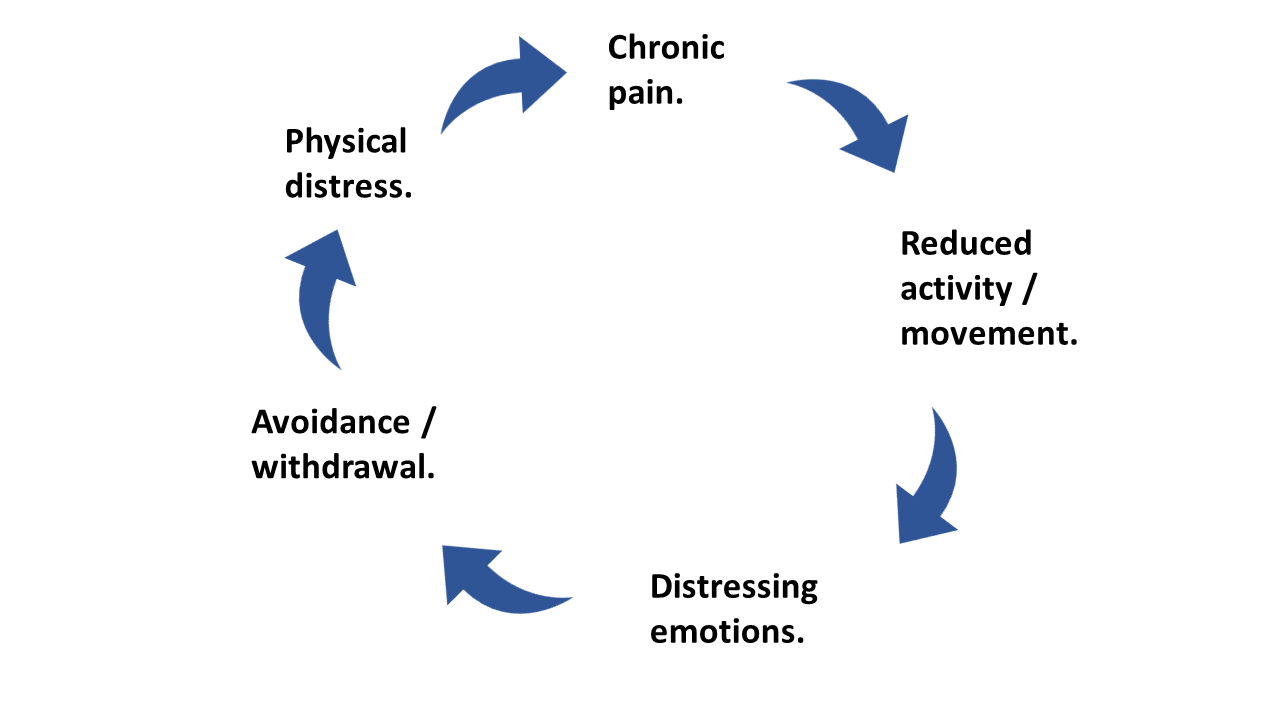
Suffering is maintained by the psychological and behavioural reactions to physical sensations of pain and that this changes acute pain into a long-term chronic condition. This diagram illustrates the vicious cycle between chronic pain, the deconditioning effects of reduced activity, negative emotions, physical avoidance and increased physical distress.
The implication of this is profound. By learning to alter the cognitive, behavioural and emotional patterns associated with the pain response, we can also alter the level of suffering and significantly improve quality of life.
What are the Key Steps in the CBT Process?
Whilst the number of sessions required to sustain a marked improvement in the management of chronic pain will depend on the findings of the initial assessment, the CBT treatment process is usually delivered over approximately 8-12 sessions as outlined below:
- Initial assessment including identification of pain thresholds and activity baselines.
- Collaborative treatment planning, including identification of personal values, choice and therapeutic goals.
- Familiarisation with the CBT treatment model and key concepts of reappraisal change and acceptance.
- Psychoeducation on the chronic pain model and development of a psychological formulation.
- Activity pacing and management of medication schedules.
- Multimodal relaxation training.
- Behavioural activation and behavioural bandwidth experiments.
- Focus of attention training and mindfulness exercises.
- Memory rescripting – particularly where trauma is implicated.
- Cognitive change and defusion techniques.
- Sleep strategies to cope with pain during sleep time.
- Relapse and resilience planning.
Each CBT treatment plan is developed around the unique pain presentation of the individual client. Clients are encouraged to collaboratively engage in the treatment planning process, to improve understanding and commitment. You can read our chronic pain article here.
To talk to a member of our team about CBT for chronic pain call +44 1732808626 or email info@thinkcbt.com